How to work with non-speaking children

What does it mean to be “Non-speaking”?
A non-speaking client is someone who does not communicate with their physiological speech system (voice). This may also mean that they use alternative means to support their message being understood by others, for example using a Speech Generating Device. This has previously been referred to as being “non-speaking”, however the term non-speaking stems from the Latin word for ‘without words’. This can often be misleading, as the person may have access to words and vocabulary but not have a physical means to express this. It is important also to identify how the client or their caregivers prefer to refer to their level of communication. Some may also prefer “minimally verbal”, meaning they have some vocalisations but cannot communicate functionally in their environment.
A client who is non-speaking may have any of the following diagnoses: Autism Spectrum Disorder, Cerebral Palsy, Down Syndrome, Selective Mutism/Mutism or any other physical or psychosocial condition that impacts their ability to communicate.
What is my role in supporting non-speaking clients?
It is important as healthcare staff to know what is best practice when working with clients who are non-speaking or minimally-verbal, and how we can build a positive relationship with them despite barriers. Additionally, as healthcare staff we should learn how to minimise these barriers by modifying the environment or attitudes of others, to enhance participation and activity outcomes. The following information will aid in helping you (therapists or AHAs) to know where to get started when preparing for a session with a non-speaking client, or communicating during ongoing sessions with a non-speaking client.
| Do | Don’t |
|---|---|
|
|
Top tips from AAC User, Noah Callan (AAC and Technology Co-ordinator, Kids Plus):
- Give plenty of time
- Don’t overlook AAC Users
- Don’t be fooled by the disability, they might be smarter than you
What types of AAC and Language Supports are there?
Light-tech
| Description | Options | Uses |
| Printed communication books or boards. Previously referred to as “low-tech”, now referred to as “light-tech” or “paper-based AAC” as it is not a lower or less important AAC tool, and is not only reserved for emergent communicators.
Often providing only limited vocabulary for learning and making simple choices. |
Core vocabulary boards
|
|
Aided language displays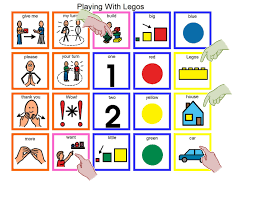 |
|
|
| PECS
|
|
|
| Visual schedules/ Choice boards
|
|
|
| First/then
|
|
Mid-tech
| Static display (not editable like an iPad screen, as it is a printed sheet) that may provide some spoken output (often recorded by someone who works with the user – ensure the recording is a voice that matches the user). | Go-Talk
|
|
| BIGMack Switch (with levels)
|
|
High-tech
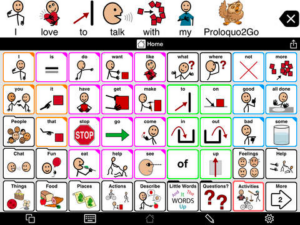
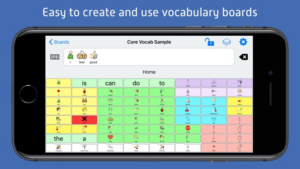
Use of an iPad or electronic device which typically has a digital voice speaking aloud, allowing access to a dynamic display and robust language system. Communication in all environments, with all communication partners.
iPad/Tablet with App
| Paid Apps | Proloquo2Go (iOS only)
LAMP Words for Life (iOS and Windows-based SGD e.g. Accent, Liberator Rugged)
Touch Chat (iOS version of WordPower)
Snap +Core First (iOS and Tobii Dynavox)
Pictello (iOS – digital story-telling for literacy and video feedback)
|
|---|---|
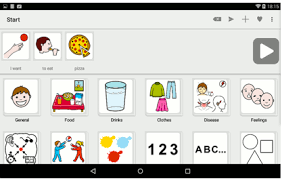
| Free Apps | Chatterboards (iOS)
Let Me Talk (iOS and Android)
SymboTalk (iOS and Android)
Sounding Board (iOS – record own voice)
|
| Dedicated Speech Generating Device (SGD) | Liberator Rugged (8” or 10”)
Accent Device (8”, 10” or 14”)
NovaChat (5”, 8”, 10” or 12”)
GridPad (12” and 15” – eye-gaze compatible)
Tobii Dynavox I-Series (eye-gaze)
|
How do I support my client who is non-speaking?
Clients who are non-speaking or minimally-verbal will either have an AAC system in place already (AAC User), or they are working with their Speech Pathologist to find the right system for them (AAC Learner). There also might be times where there is not a Speech Pathologist involved with the client, or a therapist has not yet made a recommendation for AAC. If you feel that a client will benefit from using visuals or multi-modal communication as they are presenting with minimal verbal communication, get in contact with Fora and discuss this with a therapist on the team. We can guide you through steps to take to advocate for the client to receive the care they need.
AAC User – If they already have an AAC system:
- Make sure it is with them at all times. If it’s electronic it should be charged and ready for use. If it is printed it should be easily accessible, e.g. on their desk or strapped across their body
- Gather information prior to the session to understand how they need to be supported to communicate with their device, e.g. Do they need you to model language on their AAC/device? (see modelling framework below) Can they understand what you are saying, but need time to respond? Do they need help finding less frequently used words? Do they have the skills to type words they can’t find?
- How do they like their device to be referred to? Surveys undertaken by Alyssa Hillary Zisk and Lily Konyn with people who use AAC indicated that there is a preference for certain terms among the AAC community, for example using “AAC User” or “multimodal communicator” to describe themselves, or using the term “AAC device” as opposed to “talker”. Learn about your client and what their preference is.
- Help them to pre-plan some phrases or things to say during conversations to help their participation in social conversations. This might look like planning some generic or specific phrases or questions, such as “that’s awesome!”, “no worries”, “How much will that cost?”. Maybe they want some conversation starters, or easy access to share news and stories. They may need support to manage the behaviour of speaking people such as “can you give me a minute while I write my message?”.
AAC Learner – If they are still learning how to use their AAC system, or finding the right AAC system for them:
- Refer to “Tips for using AAC” below
- Speak with a Speech Pathologist at Fora Therapy, or the therapist who might be involved with the client. The therapist might encourage you to have options available with you e.g. have apps on your iPad like Proloquo2Go or free apps like Chatterboards, Sounding Board or Choiceworks, have printed visuals like core boards, choice boards with activity options, aided language displays for specific activities, or PECS. These options would act as a trial for how the client reacts to AAC and finding an appropriate solution. You may be involved in gathering information/evidence/data for the therapist to then make the appropriate decision on AAC for the client.
- Ensure you are knowledgeable and have researched the AAC options that may be available for the client. It is okay to not have all the answers when you first meet them, and to say “I don’t know”, but it is important that you follow through with any questions that they may ask you and say “let me look into it for you”. You may then reach out to Fora or the therapist involved with the client and seek further information and help you with answering their questions.
Point about ‘being knowledgeable’:
Noah also stated that he always expected the therapist to be able to answer his questions about AAC during his AAC learning period. He wanted his therapists to have the knowledge so that he could leave knowing more about his options, rather than feeling more confused. Noah also recommended using information handouts to provide parents/carers and AAC users to further help their understanding about what AAC is and what options are available to them.
Talk to your leading Speech Pathologist at Fora – ask questions, do research, get guidance
Tips for using AAC
- Model, model, model – this is the best way for your client to become familiar with vocabulary and using the device or printed AAC as a communicative tool. Lots of repetition is key here!
- Start by modelling just the most important core words – you don’t need to model every word that you say. Important core words might be the verb or noun in the sentence e.g.
You want the water
Let’s jump together!
Make the car go! - Always model at or slightly above your AAC user’s level e.g. if they are already producing single-word utterances, model only single words or two-word combinations.
For example, little John only uses the words dog, biscuit, car independently. You would verbally say “John wants the car!” and only model on the device/with visuals “car” or “want car”.
- Start by modelling just the most important core words – you don’t need to model every word that you say. Important core words might be the verb or noun in the sentence e.g.
- Narrate what you are doing. Talk about what you are doing whilst you are playing, explore the vocabulary in the AAC option together.
Ooh you want the car to go fast! Uh-oh car stop! The car has stopped. What will happen next? Oh the car is going! - Create routines – start and end the play / session the same way each time, or sing-songs and play repetitive games to give the child an opportunity to learn the routine and then find their role in the routine.
Row, row, row your boat (visual model) gently down the stream….
Row, row, row your (expectant pause)… boat! Gently down the stream…
Modelling AAC – Prompting Hierarchy
From least to most support
| Expectant Pause | Give the child time to respond or the opportunity to initiate communication |
| Indirect Nonverbal Prompt | Use your body language to indicate to the child that something is expected (e.g. expectant facial expression, questioning hand motion with a shrug etc). |
| Indirect Verbal Prompt | Use open ended questions that tells the child that something is expected but nothing too specific (e.g. “Now what?” “what should we do next?”). |
| Request a Response | You can direct the child to a more specific response (e.g. “Tell me what you want”) or offer the child a choice between two objects (pictured below).
|
| Gestural Cue | You can point to the symbol or leave/tap your finger there for several seconds to get the child started with their message. |
| Partial Verbal Prompt | Give them part of the expected response (e.g. “You went to the….”). |
| Direct Model | Model on the students device (e.g. “the bear is sad”). Pause and wait for the child to imitate or respond. |
| Physical Assistant
NOTE: It is encouraged that whenever you are using physical prompting, that you coach the parent/caregiver to provide this level of prompting as the client will be most comfortable with them physically touching them. Only initiate physical prompting if; a) you feel you have a good rapport with the client and b) you have sought permission from the client and the caregiver, or informed the client before you touch them that you are about to do so. |
Provide hand over hand assistance to help the child to form the message using their device
Elbow Prompt (nudge)
Hand-under-hand Prompt
Hand-over-hand Prompt
|
Additional resources
For additional information and resources you can use in therapy, see these materials:
- AAC Training Guide
- Activity Choice Board (with Core Vocab)
- Department of Education – How to Talk to a Student with ASD
- Department of Education – How to Use Visual Supports
- First / Then Visual
- Playdough Activity Board (PODD)
- Project Core (PCS) Core Word Board
- Proloquo2go – Core Board
- SPA Handout for AAC
Shannon
Fora's Speech Pathology team